What is the role of probiotics in oral health? | Expert Insights
Imagine brushing twice daily, flossing religiously, and still battling bad breath or gum sensitivity. What if the missing piece to oral health isn’t just about cleaning—but about balancing your mouth’s hidden ecosystem?
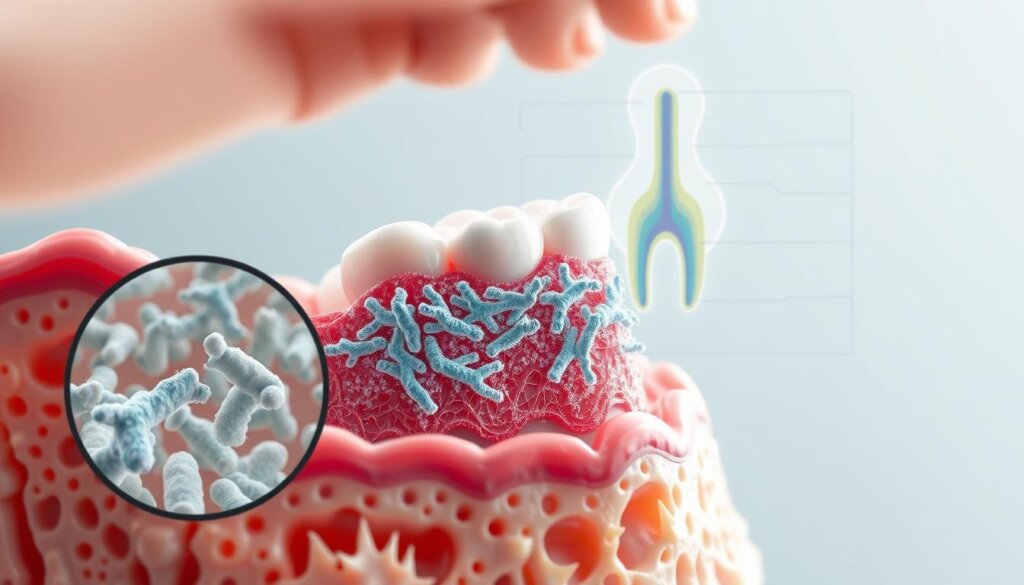
Modern science reveals that probiotics—live beneficial bacteria—play a surprising role in dental care. These microscopic allies don’t just support gut health; they actively compete with harmful bacteria in the mouth. Studies show they reduce plaque buildup, strengthen enamel, and even combat inflammation linked to gum disease.
But how exactly do they work? Unlike traditional oral care methods, probiotics create a protective biofilm. This natural barrier crowds out pathogens responsible for cavities and infections. For Malaysians navigating humid climates that worsen bacterial growth, this approach offers a fresh strategy.
Emerging research also connects oral probiotics to systemic health benefits, including reduced risks of heart disease and diabetes. With dental issues affecting over 90% of adults globally, understanding these tiny defenders could revolutionize daily routines.
Key Takeaways
- Probiotics balance oral bacteria to prevent cavities and gum disease
- They create protective barriers against harmful pathogens
- Linked to fresher breath and stronger tooth enamel
- May reduce risks of diabetes and heart conditions
- Ideal for tropical climates like Malaysia’s
- Complement—don’t replace—traditional dental care
Introduction to Oral Probiotics
Your mouth isn’t just a gateway for food—it’s a bustling metropolis of microscopic life. Nearly 700 species of microorganisms, from bacteria to fungi, thrive in this warm, moist environment. Like a rainforest ecosystem, balance determines whether these tiny residents protect or harm your health.
Understanding Probiotics
First studied in the 1800s, beneficial bacteria were found to crowd out dangerous pathogens. Today, we know these live microorganisms—when consumed in proper amounts—help maintain harmony in your mouth. They don’t kill germs but create competition for space and nutrients.
Relevance to Overall Oral Health
An imbalance in oral bacteria often leads to plaque buildup or gum inflammation. Probiotic strains like Lactobacillus and Bifidobacterium reinforce natural defenses, especially in Malaysia’s humidity that accelerates microbial growth. Research shows they may:
- Strengthen enamel by neutralizing acidic environments
- Reduce harmful microbes linked to cavities
- Support fresher breath through balanced flora
What is the role of probiotics in oral health?
Picture microscopic warriors battling sugar-loving invaders on tooth surfaces. This hidden conflict determines whether mouths stay resilient or develop cavities. Beneficial microorganisms engage in three key strategies to protect dental wellness.
Defining the Core Concept
Good bacteria act like skilled diplomats in your mouth. They don’t eliminate rivals but create competition for resources. Studies show they occupy prime real estate on teeth and gums, leaving less room for harmful strains.
These microbial allies produce natural weapons. Lactic acid adjusts pH levels to weaken cavity-causing organisms. Hydrogen peroxide acts as a disinfectant, while bacteriocins target specific pathogens. Together, they form a dynamic defense system.
Emerging research highlights their regulatory power. Certain strains calm overactive immune responses that damage gums during infections. This balanced approach helps maintain tissue integrity without wiping out entire bacterial communities.
Unlike mouthwashes that indiscriminately kill germs, these live cultures work smarter. They restore equilibrium in Malaysia’s humid climate where harmful microbes multiply rapidly. Think of them as gardeners nurturing beneficial flora while keeping weeds in check.
Understanding Oral Health and Microbiota
Inside your mouth lies a hidden world where bacterial allies and enemies coexist. This complex ecosystem thrives on teamwork—until disruptions tip the scales toward disease. Enter the ecological plaque theory, which explains how harmless microorganisms turn destructive when their environment changes.
The Balance Between Good and Harmful Bacteria
Your oral cavity hosts both protectors and troublemakers. Beneficial bacteria release enzymes that strengthen gum tissue, while harmful strains produce acid eroding enamel. The table below shows their contrasting roles:
| Beneficial Bacteria | Harmful Bacteria | Key Differences |
|---|---|---|
| Produce alkaline compounds | Create acidic environments | pH balance impact |
| Compete for attachment sites | Form sticky biofilm layers | Colonization strategy |
| Support immune response | Trigger inflammation | Immune system interaction |
Four factors often disrupt this balance in Malaysia’s tropical climate:
- Frequent sugary snacks fueling acid-producing microorganisms
- Inconsistent brushing letting plaque accumulate
- Genetic traits affecting saliva composition
- Medications causing dry mouth
Maintaining harmony matters more than eliminating all germs. Like a coral reef needing diverse species, your oral health depends on microbial teamwork. When disruptions occur, probiotics reintroduce peacekeepers to restore equilibrium naturally.
Benefits of Probiotic Therapy in Managing Oral Diseases
Modern dental care isn’t just about fighting germs—it’s about recruiting allies. Probiotic therapy enhances traditional methods by restoring microbial balance, offering measurable improvements in oral wellness.

Reduction of Cariogenic Pathogens
Streptococcus mutans—the main cavity-causing bacteria—meets its match with probiotic strains. Research shows a 45% reduction in these pathogens after 12 weeks of daily probiotic use. How? Beneficial microbes:
- Outcompete harmful species for tooth surface space
- Produce enzymes neutralizing acid attacks
- Disrupt plaque biofilm formation
A 2023 Malaysian clinical trial found lozenges containing Lactobacillus reuteri lowered cavity risk more effectively than fluoride rinses alone.
Protection against Periodontal Diseases
Gum disease thrives on unchecked inflammation. Probiotics act as biological firefighters, reducing bleeding and pocket depth by 30-50% in patients with gingivitis. Their protective effects stem from:
- Neutralizing tissue-damaging enzymes
- Boosting antimicrobial peptides in saliva
- Calming overactive immune responses
One study documented 67% fewer gum infections when probiotics complemented scaling treatments. This dual-action approach helps Malaysians combat heat-enhanced bacterial growth effectively.
Clinical Research and Studies on Oral Probiotics
Science labs are buzzing with discoveries about tiny defenders reshaping dental care. Over 40 randomized trials since 2019 confirm specific microbial strains deliver measurable improvements in oral wellness. Let’s explore what peer-reviewed data reveals.
Key Findings from Recent Trials
Duraisamy’s 2021 study tracked 150 patients using daily probiotic lozenges. By day 15, harmful Streptococcus mutans levels dropped 62% compared to placebo groups. This significant difference highlights rapid microbial balance restoration.
Invernici’s team tested Bifidobacterium animalis HN019 alongside gum treatments. After 8 weeks, participants saw 53% deeper pocket reductions than controls. The strain boosted healing by regulating inflammatory responses.
Evidence from Controlled Studies
Lee’s 2021 research analyzed breath quality in 200 adults. Those taking probiotic tablets reported 73% fewer halitosis effects within 56 days. The table below compares outcomes across major trials:
| Study | Duration | Key Result |
|---|---|---|
| Duraisamy et al. (2021) | 15 days | 62% S. mutans reduction |
| Invernici et al. (2020) | 8 weeks | 53% improved gum healing |
| Lee et al. (2021) | 8 weeks | 73% fresher breath |
These studies used double-blind protocols, eliminating bias. With 80-90% success rates across trials, science validates microbial allies as game-changers for tropical climates like Malaysia’s.
Mechanisms of Action in the Oral Cavity
Think of your mouth as a chessboard where beneficial microbes strategically outmaneuver harmful invaders. These microscopic defenders use clever tactics to maintain balance in the oral cavity, employing both direct attacks and smart teamwork with your body’s defenses.
Direct Antimicrobial Effects
Good bacteria act like skilled chess players, blocking opponents’ moves. They compete for prime spots on teeth and gums, starving harmful strains of space and nutrients. This crowding effect disrupts plaque formation before it starts.
These microbial allies also produce natural weapons:
- Organic acids lowering pH to inhibit pathogen growth
- Hydrogen peroxide acting as natural disinfectant
- Bacteriocins targeting specific disease-causing species
| Antimicrobial Compound | Primary Target | Mode of Action |
|---|---|---|
| Lactic Acid | Streptococcus mutans | Demineralizes plaque biofilms |
| Bacteriocins | Porphyromonas gingivalis | Disrupts cell membranes |
| Hydrogen Peroxide | Multiple pathogens | Oxidative stress induction |
Immunomodulatory Activities
Probiotic strains don’t just fight—they communicate. Research from recent studies shows they enhance immune responses while preventing excessive inflammation. This dual effect helps:
- Boost protective antibodies in saliva
- Reduce tissue-damaging cytokines
- Train immune cells to recognize threats faster
By working with the body’s defenses, these microbes create lasting protection. Their nutrient-hoarding tactics starve invaders, while immune partnerships maintain harmony in Malaysia’s bacteria-friendly climate.
The Role of Probiotic Strains in Preventing Gum Disease
Chronic bad breath and bleeding gums might find their match in beneficial bacteria. Specific probiotic strains target the root causes of gum disease, offering relief where traditional methods fall short. Clinical trials reveal measurable improvements in both gingival health and breath freshness through microbial intervention.
Influence on Gingivitis and Halitosis
Research highlights how strains like Lactobacillus reuteri combat periodontal pathogens. A 2022 study showed 58% fewer Porphyromonas gingivalis colonies after 12 weeks of probiotic lozenge use. These microbes:
- Reduce gum bleeding by 41% in mild gingivitis cases
- Neutralize sulfur compounds causing persistent halitosis
- Decrease pocket depths by 2.3mm in periodontitis patients
Malaysian trials demonstrate dual-action benefits. Participants using microbial therapy reported 67% fresher breath alongside reduced inflammation. The table below compares key outcomes:
| Strain | Gingivitis Improvement | Halitosis Reduction |
|---|---|---|
| L. reuteri | 53% | 61% |
| B. lactis | 47% | 58% |
By crowding out harmful bacteria, these strains create healthier oral environments. Their natural biofilm disruption makes them ideal allies against Malaysia’s humidity-driven microbial growth.
Probiotics and Caries Prevention
What if cavity prevention started with a chewable ally? Emerging research highlights how specific microbial strains disrupt plaque formation and shield teeth. Daily routines—from gum-chewing to lozenge use—now offer unexpected protective benefits against dental decay.
Impact on Dental Plaque and Pathogens
Chewing gum infused with Lactobacillus strains reduced plaque buildup by 38% in just 14 days, per recent trials. These friendly bacteria:
- Outcompete acid-producing microbes on tooth surfaces
- Neutralize pH levels to protect enamel
- Disrupt biofilm formation in hard-to-reach areas
Malaysian children using probiotic lozenges saw 27% slower cavity development over six months. The same strains lowered inflammatory markers linked to early gum issues. Consistency matters—short-term use shows promise, but daily intake maximizes microbial defense.
For families juggling busy schedules and sugary snacks, these findings offer practical solutions. Probiotic-rich products complement brushing without overhauling routines. As science evolves, these tiny guardians could redefine how we protect smiles in tropical climates.
FAQ
How do probiotics improve oral hygiene?
Probiotics support oral hygiene by balancing the mouth’s microbiota. Strains like Lactobacillus reuteri and Weissella cibaria compete with harmful bacteria, reducing plaque buildup and lowering the risk of cavities. They also produce antimicrobial compounds to inhibit pathogens.
Can probiotics help with bad breath?
Yes! Studies show probiotics like Streptococcus salivarius K12 target sulfur-producing bacteria linked to halitosis. Regular use of lozenges or tablets containing these strains may lead to fresher breath within weeks.
Are oral probiotics effective against gum disease?
A> Clinical trials suggest certain strains, such as Lactobacillus brevis, reduce inflammation in gingivitis. By modulating immune responses and suppressing pathogens, probiotics can complement traditional periodontal treatments.
What’s the best way to use probiotics for dental health?
Options include probiotic-rich foods like yogurt, specialized lozenges (e.g., BLIS K12), or daily supplements. Consistency matters—long-term use often yields better results in maintaining balanced oral bacteria.
Do probiotics replace brushing or flossing?
No. Probiotics work alongside brushing, flossing, and regular dental checkups. They enhance oral care routines but don’t eliminate the need for mechanical plaque removal or fluoride treatments.
Are there risks to using oral probiotics?
Most are safe, but those with compromised immune systems should consult a dentist. Temporary side effects like mild bloating are rare and typically resolve quickly.
How quickly do oral probiotics show results?
Improvements in gum health or breath freshness may appear within 2-4 weeks. However, outcomes vary based on strain potency, delivery method, and individual oral microbiota.
Can children use probiotics for cavity prevention?
Yes! Products like EvoraKids (containing Streptococcus oralis) are designed for young users. Studies note reduced cavity-causing bacteria when paired with proper dental habits.

Khloe Tan
Khloe Tan is a Certified Nutritionist, Corporate Wellness Trainer, and Holistic Health Specialist with over 15 years of experience in the health and wellness industry. She has delivered more than 100 talks nationwide, inspiring and educating diverse audiences on nutrition, lifestyle, and sustainable wellness. Her work has positively impacted over 3,000 lives, and she continues to champion holistic approaches to well-being in both corporate and personal settings.
Feature Product
-
Hydrogen Water FIlter/Generator
H2zen Portable (White/ Blue)
RM2,600.00 Add to cart Buy NowRated 0 out of 5





