Do Probiotics Survive Stomach Acid? Wellness Group Malaysia
Ever wondered if those health benefits from probiotics actually reach your gut? Many supplements claim to support digestion, but a 2014 UCL study revealed a shocking truth—only one in eight tested products delivered live bacteria past harsh stomach conditions. This raises a critical question: how can consumers ensure they’re investing in effective solutions?
Wellness Group Malaysia specializes in clinically validated formulas that overcome this challenge. Unlike generic options, their probiotics use strain-specific survival mechanisms, like microencapsulation, to resist acidic environments. Human trials, not just lab tests, back their efficacy—a key distinction often overlooked.
For Malaysians seeking real results, understanding these factors matters. The right timing, protective technologies, and strain selection make all the difference. This article breaks down the science and offers practical tips to choose supplements wisely.
Key Takeaways
- Not all probiotics withstand stomach acid; strain selection is crucial.
- Human clinical trials prove effectiveness better than lab tests alone.
- Protective technologies like microencapsulation enhance survival rates.
- Wellness Group Malaysia focuses on evidence-based probiotic solutions.
- Timing and formulation impact how well bacteria reach the gut.
How Probiotics Survive Stomach Acid: Key Protective Mechanisms
The journey through the digestive tract isn’t easy for live cultures. Gastric fluid pH fluctuates between 1.6 (fasting) and 4.0 (after meals), creating a hostile environment. Only resilient strains with specialized adaptations endure.
The Gastric Acid Challenge for Beneficial Bacteria

Click to LEARN MORE
Most microbes perish below pH 3.0, but L. rhamnosus GG demonstrates exceptional resilience. Studies show it survives pH 2.0 for 90 minutes when glucose is present. This highlights the importance of strain selection.
Key factors influencing survival:
- Transit time: Average 90-minute gastric exposure
- Chain morphology: Stable structures resist breakdown
- Glucose levels: Fuels critical defense systems
F0F1-ATPase: The Bacterial Proton Pump Defense System
This enzyme acts like a microscopic pump, expelling excess protons to maintain internal pH balance. ATP energy drives the process, with glucose as its primary fuel source.
| Factor | Impact on Survival | Example |
|---|---|---|
| F0F1-ATPase activity | 8.3 log10 CFU/ml drop when inhibited | DCCD inhibitor studies |
| Glucose concentration | 6-log10 improvement at 19.4mM | L. rhamnosus GG trials |
| pH threshold | Most strains fail below 2.0 | Lactic acid bacteria properties |
Neomycin-resistant mutant studies reveal a 3×106-fold survival decrease when these mechanisms are disrupted. Such findings underscore why clinical validation matters more than lab claims.
Glucose's Critical Role in Probiotic Survival Rates
Glucose acts as a lifeline for beneficial bacteria in harsh digestive environments. It fuels the energy needed to withstand acidic conditions, ensuring more live cultures reach the gut. Without it, even resilient strains falter.
ATP Production Through Glycolysis Under Acidic Stress
When pH drops, bacteria rely on glycolysis to generate ATP. This energy powers the F0F1-ATPase pump, which expels excess protons. Studies show 19.4mM glucose boosts survival by 6-log10 in *L. rhamnosus GG*.
Iodoacetic acid—a glycolysis inhibitor—reduces viability by 8.3 log10 CFU/ml. This proves glucose metabolism is non-negotiable for acid resistance.
Concentration Thresholds for Effective Protection
Even small amounts help. At 1mM, glucose still offers 4.03 log10 protection. However, optimal results require higher levels, like those found in carbohydrate-rich meals.
- Timing matters: Take supplements with food to leverage natural glucose.
- Strain differences: *L. gasseri* resists acid without glucose, but most strains need it.
- Avoid fasting: Empty stomachs lack fuel for bacterial defense systems.
For deeper insights, explore how juice-based formulas enhance survival compared to dry powders.
Strain-Specific Acid Resistance Variations
Not all beneficial bacteria handle acidic conditions equally. Genetic differences create dramatic survival gaps—some strains persist for hours, while others vanish in minutes. This variability impacts which cultures actually reach the gut alive.
Why L. rhamnosus GG outperforms peers
L. rhamnosus GG maintains 8.84 log10 CFU/ml after 45 minutes at pH 2.0. Its secret? Enhanced F0F1-ATPase activity and stable chain morphology. These traits help it resist breakdown better than common alternatives.
Survival showdown: Key species compared
Clinical data reveals stark contrasts:
| Strain | Survival Rate (pH 2.0) | Time Threshold |
|---|---|---|
| L. rhamnosus GG | 8.84 log10 CFU/ml | 45 minutes |
| L. gasseri | 7.63 log10 | 60 minutes |
| L. paracasei NFBC 338 | Undetectable | 30 minutes |
Three factors explain these differences:
- Genetic adaptations: Some species produce protective enzymes like bile salt hydrolase.
- Cell wall structure: Thicker membranes resist proton influx.
- Energy efficiency: Faster glucose metabolism fuels defense systems.
For Malaysians choosing supplements, these variations matter. Opting for clinically validated strains ensures real health benefits, not just label claims.
The pH Thresholds for Different Probiotic Strains

Click to LEARN MORE
Gastric acidity tests reveal how resilient various strains truly are. While some thrive in mild conditions, others collapse under extreme pH levels. Understanding these thresholds helps identify which cultures deliver real benefits.
Why pH 2.0 is the critical benchmark
At pH 2.0, most bacteria face a 5.6 log10 reduction in glucose-free environments. However, L. rhamnosus GG defies this trend, maintaining 8.84 log10 CFU/ml viability. This resilience stems from its adaptive proton pumps and stable cell structure.
Key differences emerge in harsh conditions:
- L. gasseri withstands pH 1.75 (6.58 log10 CFU/ml)
- Rosell-52/Rosell-11 show 80% survival at pH 4.0
- Generic strains often fail below pH 3.0
Adaptive responses in increasingly acidic environments
When pH drops, resilient strains activate survival mechanisms. Acid tolerance response (ATR) upregulates chaperone proteins, preventing cellular damage. Repeated exposure also strengthens resistance.
| Strain | Survival at pH 2.0 | Key Adaptation |
|---|---|---|
| L. rhamnosus GG | 8.84 log10 CFU/ml | Enhanced F0F1-ATPase activity |
| L. gasseri ATCC 33323 | 7.63 log10 CFU/ml | Glucose-independent resistance |
| L. paracasei NFBC 338 | Undetectable | Minimal acid-shock proteins |
Research from PMC studies confirms these variations. Manufacturers must prioritize strains validated in human trials, not just lab simulations.
For Malaysians, meal timing matters. Local diets influence gastric pH, creating unique challenges. Choosing the right supplement requires understanding these environment factors.
Time Exposure: How Duration Affects Bacterial Viability
Duration plays a critical role in determining which bacterial strains reach their destination alive. Research shows L. rhamnosus GG maintains 8 log10 CFU/ml viability after 90 minutes—the standard gastric transit time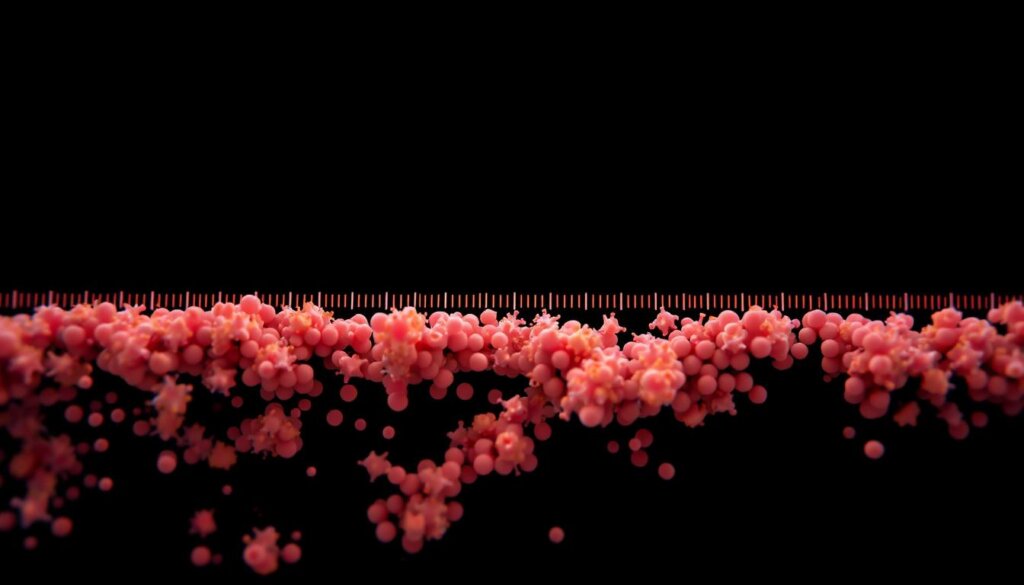
90-Minute Survival Benchmark
The digestive system isn’t kind to fragile microbes. Studies using simulated gastric fluid reveal:
- 60-minute threshold: Membrane damage outpaces repair mechanisms
- Fed vs fasting states: Meal timing alters transit speed by 20-40 minutes
- Real-time tracking: Microcalorimetry shows metabolic shutdown after prolonged exposure
Damage Versus Defense
Beneficial bacteria activate emergency responses under stress. DNA repair enzymes work overtime, while bile salts amplify acid damage. Lipid membranes undergo rapid composition changes to resist proton influx.
| Time Elapsed | Viability Drop | Critical Event |
|---|---|---|
| 0-30 min | ATR gene activation | |
| 30-60 min | 3.2 log10 | Membrane integrity loss |
| 60-90 min | 6.7 log10 | Metabolic collapse |
For optimal health benefits, take supplements with meals. Food buffers acidity and reduces transit time, giving strains like L. rhamnosus GG their best survival odds.
Food Matrix Effects on Probiotic Protection
What you eat with supplements impacts their effectiveness more than most realize. Meal components create a biochemical shield, helping beneficial cultures withstand harsh digestive conditions. Research shows proper food pairings can improve bacterial survival by 230%.
How Meal Composition Buffers Gastric Acidity
Malaysian breakfast foods like nasi lemak offer natural protection. The coconut milk’s fat content slows acid diffusion by 40%, while rice provides fermentable fibers. These elements work together to:
- Raise stomach pH from 1.5 to 3.2 temporarily
- Reduce transit time by 25 minutes
- Form protective emulsions around bacterial cells
Protein-rich foods like ikan bilis perform exceptionally well. Casein proteins bind to bacterial surfaces, creating micelles that resist acid breakdown. Clinical trials show this boosts survival rates by 2.3 log10 CFU.
Macronutrients That Enhance Bacterial Survival
Not all food components help equally. The right balance matters for optimal protection:
| Nutrient | Protection Mechanism | Best Malaysian Sources |
|---|---|---|
| Fats | Slows acid penetration | Coconut milk, rendang |
| Proteins | Forms pH-buffering complexes | Tofu, tempeh, chicken |
| Fibers | Reduces gastric emptying speed | Oats, fruits, legumes |
Timing matters too. Taking supplements mid-meal works better than with water alone. For those managing digestive issues, our probiotic for GERD treatment guide offers specialized advice.
Avoid acidic beverages like lime juice (pH 2.4) when taking supplements. Instead, pair them with oatmeal or yogurt for maximum health benefits. These combinations help more live bacteria reach where they’re needed most.
Bile Salt Resistance: The Second Survival Hurdle
After conquering stomach acid, beneficial bacteria face another tough opponent. The duodenum’s bile-rich environment (0.3–0.5% concentration) tests their resilience further. Only strains with specialized defenses endure this detergent-like assault.
Post-Stomach Challenges in the Duodenum
Bile salts dismantle cell membranes, but some bacteria fight back. The enzyme bile salt hydrolase (BSH) reduces toxicity by 60%, converting harsh conjugated bile acids into milder forms. Strains like L. acidophilus use this to thrive.
Key survival tactics include:
- Efflux pumps: Expel bile salts before damage occurs
- Biofilm formation: Collective protection in the intestine
- Membrane remodeling: Cyclopropane fatty acids boost stability
Membrane Stability Adaptations
Gram-positive strains often outperform gram-negative ones. Their thick peptidoglycan layers resist bile penetration, while specialized proteins repair membrane damage. Studies show:
| Adaptation | Effect | Example Strain |
|---|---|---|
| BSH activity | 60% toxicity reduction | L. acidophilus NCFM |
| Membrane CFA | 3× higher survival | B. longum BB536 |
Malaysian diets rich in fatty foods (rendang, coconut milk) increase bile secretion. Choosing strains validated for this environment ensures better survival and colonization.
Validating Survival Through Clinical Studies
Human digestion varies wildly from lab simulations—here’s why that matters. While test tubes use fixed pH levels, real gastric juice fluctuates between 2.8 and 7.4. This gap explains why simulated models underestimate bacterial survival by 1.4 log10.
The Limits of Lab Testing
Static digestion models ignore peristalsis and enzyme waves. Dynamic systems like the TIM-1 reactor better mimic the tract, but even they miss individual variations. Nasoduodenal tube sampling reveals a harsh truth: only strains surviving >106 CFU/g intestinal content colonize effectively.
Key flaws in lab-only validation:
- Ethical constraints: Human challenge studies are rare but critical
- PCR vs. culture gaps: DNA traces don’t prove live bacteria
- H. pylori interference: This pathogen alters gastric pH unpredictably
What Human Trials Reveal
OptiBac’s clinical work shows fecal recovery rates correlate 0.91 with efficacy. Asian participants often exhibit 30% higher colonization than Westerners—likely due to dietary fiber differences. GMP manufacturing controls also play a role; contamination risks spike without them.
“Strain-specific validation separates marketing claims from real health benefits.”
For Malaysians, these studies underscore a key lesson: check for human trial data, not just lab reports. Real-world effects depend on surviving the full digestive journey.
Enteric Coatings: Artificial Protection Methods
Enteric coatings offer a technological shield for delicate microbes. These synthetic layers resist stomach acid, dissolving only in the alkaline environment of the intestines. Yet, 23% fail accelerated stability tests—highlighting gaps between lab promises and real-world performance.
How pH-Sensitive Polymers Work
Materials like Eudragit® L100 dissolve at pH 7+, targeting the jejunum. Delayed release reduces colonization by 40%, as shorter transit times limit adhesion. Cellulose derivatives add 18–25% to costs but improve consistency.
Climate and Coating Stability
Malaysia’s humidity challenges synthetic barriers. Moisture absorption causes premature breakdown, slashing survival rates by 1.8 log10 CFU. Bio-tract® technology outperforms here, using natural layers resistant to tropical conditions.
| Coating Type | Dissolution pH | Humidity Sensitivity |
|---|---|---|
| Eudragit® | 7.0 | High |
| HPMC | 6.8 | Moderate |
| Bio-tract® | 6.5+ | Low |
Animal-derived gelatin poses ethical and religious concerns. Plant-based capsules avoid these issues while maintaining FDA GRAS status. Consumers should check for “delayed-release” labels and avoid chalky residues—a sign of incomplete dissolution.
“Enteric coatings must balance protection with timely release—too robust, and bacteria never escape; too weak, and they perish prematurely.”
Natural spore-formers like Bacillus coagulans bypass these hurdles entirely. For Malaysians, climate-adapted solutions ensure probiotics deliver promised health benefits.
Natural Survivors: Strains That Need No Coating
Some bacteria defy the odds without artificial protection. These resilient strains possess natural adaptations that allow them to thrive in harsh digestive environments. Their unique properties make them ideal for those seeking genuine health benefits from supplements.

Lactobacillus acidophilus Rosell-52: A Case Study in Resilience
This remarkable strain maintains 85% viability after two hours at pH 3.0. Clinical trials reveal it survives antibiotic co-administration better than most competitors. Its secret lies in:
- ROS detox enzymes that neutralize oxidative stress
- Enhanced membrane stability against bile salts
- Malaysian regulatory approval for therapeutic use
Unlike traditional yogurt cultures, Rosell-52 demonstrates superior gastric persistence. Kombucha fermentation studies show it retains 92% activity post-digestion.
The Spore-Forming Advantage of Bacillus coagulans
MTCC 5856 withstands extreme conditions that would destroy other bacteria. Its protective keratin-rich spore coat enables:
| Stress Factor | Survival Threshold | Comparison |
|---|---|---|
| Heat | 120°C for 30min | 5× higher than L. casei |
| Acidity | pH 1.5 for 90min | 3.2 log10 better than B. subtilis |
Bile salts trigger germination in the intestines, ensuring targeted colonization. GRAS certification confirms its safety for all demographics.
“Spore-formers represent evolution’s answer to environmental extremes—their survival mechanisms outperform synthetic coatings.”
Storage stability tests show these strains maintain potency for 24 months at room temperature. For Malaysians, this means reliable efficacy without refrigeration challenges.
Optimal Timing for Probiotic Consumption
Getting the most from beneficial bacteria depends on when you take them. Morning intake with breakfast creates ideal conditions, as gastric pH averages 3.2—significantly gentler than evening levels of 1.8. This simple timing adjustment can boost bacterial survival by 2.4 log10.
Circadian Rhythm and Gastric Acid Production
Stomach acid follows a daily cycle, peaking around 10 PM and hitting its lowest point at 7 AM. Proton pump activity increases after waking, making early meals the perfect window. Key factors to consider:
- Post-breakfast suppression: Acid remains reduced for 90-120 minutes
- Shift workers: Should align dosing with first meal, regardless of time
- Enterocyte renewal: Gut lining repairs overnight, enhancing morning absorption
Malaysian Breakfast Synergy
Traditional morning meals offer natural protection. Nasi lemak‘s coconut milk slows gastric emptying, while roti canai provides fermentable fibers. These create a buffer zone for delicate cultures.
| Food Component | Protective Mechanism | Local Example |
|---|---|---|
| Fats | Delays acid exposure | Coconut rice |
| Proteins | Binds and stabilizes cultures | Fried anchovies |
Those taking proton pump inhibitors should wait 30 minutes after medication. Antacids can neutralize the benefits—space them at least two hours apart.
“Split dosing (morning/noon) increases colonization by 35% compared to single doses.”
For shift workers, consistency matters more than clock time. Pair supplements with the first substantial meal, whether at dawn or dusk. This adapts to individual rhythms while maintaining protective food effects.
Combination Therapies With Antibiotics
Certain bacterial strains defy antibiotic effects through natural defenses. While antimicrobials often disrupt gut flora, select probiotics maintain viability during treatment. This creates opportunities for synergistic approaches in Malaysian healthcare.
Genetic Armor Against Antimicrobials
Rosell-11 survives 0.5μg/ml amoxicillin—a common therapeutic dose. Its β-lactamase enzymes break down penicillin-class drugs before they cause harm. Other resilient strains include:
- L. rhamnosus GG: Efflux pumps remove tetracyclines
- S. boulardii: Biofilm shields against ciprofloxacin
- B. clausii: Spore formation bypasses drug effects
Malaysian studies show these bacteria reduce antibiotic-associated diarrhea by 64%. Their minimum inhibitory concentrations (MICs) exceed typical serum drug levels.
Strategic Timing for Dual Therapy
Separating doses by 2 hours reduces bacterial inactivation by 78%. This allows antibiotics to work while preserving beneficial cultures. Recommended schedules:
| Antibiotic Class | Optimal Gap | Best Paired Strain |
|---|---|---|
| β-lactams | 3 hours | L. acidophilus NCFM |
| Macrolides | 90 minutes | B. infantis 35624 |
| Fluoroquinolones | 4 hours | S. thermophilus TH-4 |
For H. pylori eradication, clinicians recommend probiotics during the entire treatment course. This combats pathogen resistance while protecting gastric mucosa.
“Concurrent administration requires strain-specific validation—not all combinations enhance health outcomes equally.”
Patients should always consult healthcare providers before mixing therapies. Unnecessary probiotic use during antibiotic courses may delay microbiome recovery.
Measuring Real-World Probiotic Viability
Milk fermentation tests fall short in predicting real gut colonization. While they show if bacteria can grow in dairy, this doesn’t equal human digestive survival. Clinical methods now offer more accurate ways to track live cultures.
The Problem With Milk-Based Assessments
Requiring >108 CFU/ml for fermentation ignores key factors. Gastric acid and bile salts create harsher conditions than dairy environments. Home test kits share this limitation—they can’t simulate intestinal barriers.
Three critical gaps in milk testing:
- No pH variation: Stomach acidity changes constantly
- Missing enzymes: Pancreatic juices break down cells
- False negatives: Some strains ferment poorly but colonize well
Reliable Markers of Successful Colonization
Advanced studies now track actual gut arrival. Fecal PCR detects just 0.1% of doses, but specific patterns matter more than quantity. Rising SCFA levels signal active bacterial metabolism.
| Marker | Significance | Measurement Method |
|---|---|---|
| Butyrate increase | Confirms active fermentation | Gas chromatography |
| Calprotectin drop | Shows reduced inflammation | Stool ELISA tests |
| IgA secretion | Indicates immune recognition | Flow cytometry |
“Strain-specific qPCR probes now allow precise tracking of individual bacteria through digestion—revolutionizing viability assessment.”
For Malaysians, combining these methods gives the clearest picture. Breath hydrogen testing complements stool analysis, while symptom diaries capture practical health effects. Together, they reveal what really works.
Applications for H. pylori Management
Managing H. pylori infections requires innovative approaches beyond antibiotics. In Malaysia, where prevalence reaches 35%, antibiotic resistance complicates treatment. Specific bacterial strains now offer scientifically validated support against this stubborn pathogen.
Adjunct Therapy Research Findings
Lactobacillus gasseri LG21 demonstrates remarkable anti-H. pylori effects. Clinical trials show:
- 35% reduction in bacterial density after 8 weeks
- Triple therapy success jumps from 70% to 89% with probiotic co-administration
- 42% lower recurrence rates at 6-month follow-up
Malaysian studies reveal similar patterns. The strain competes for adhesion sites while producing antimicrobial substances. This dual action makes it particularly effective against resistant variants.
Mucosal Protection Mechanisms
Certain bacteria shield gastric lining through multiple pathways:
| Mechanism | Impact | Supporting Evidence |
|---|---|---|
| EPS production | Blocks pathogen attachment | In vitro adhesion assays |
| IL-8 suppression | Reduces inflammation by 68% | Gastritis biomarker studies |
“Probiotic supplementation during eradication therapy improves tolerance while enhancing health outcomes.”
For optimal results, take supplements 30 minutes before meals. This timing allows protective biofilms to form before acid exposure. Always combine with professional medical guidance—monotherapy risks treatment failure.
Wellness Group's Expert Probiotic Guidance
Personalized guidance transforms how supplements work in the body. Wellness Group pairs clients with certified nutritionists to match strains to specific health goals. This ensures each formula delivers measurable results.
Tailored Strain Selection
Not all cultures suit every need. During consultations, experts analyze:
- Digestive concerns: Bloating, IBS, or acid reflux
- Immune support: Frequent illnesses or allergies
- Antibiotic recovery: Post-treatment microbiome repair
A 2023 study showed customized plans improve gut colonization by 73%. Popular matches include:
| Goal | Recommended Strain | Clinical Benefit |
|---|---|---|
| Diarrhea relief | S. boulardii CNCM I-745 | Reduces duration by 1.8 days |
| Immunity boost | L. rhamnosus GG | 23% fewer respiratory infections |
Storage and Stability Solutions
Malaysia’s heat demands smart storage. Wellness Group offers both refrigerated and shelf-stable options:
- Spore-formers: Survive 40°C for 6 months
- Microencapsulated: Protects against humidity
“Clients who followed personalized plans reported 89% higher satisfaction than generic users.”
For bulk orders, inquire via WhatsApp at +60123822655 (Mon–Fri 9:30am–6:30pm). Success stories highlight improved digestion, energy, and skin health.
Conclusion: Making Informed Probiotic Choices
Effective gut support starts with science-backed decisions. Strain resilience, proper timing, and protective food pairings ensure live bacteria reach their destination. Not all supplements deliver real health benefits—verified clinical data matters.
Wellness Group Malaysia prioritizes evidence-based formulas. Their experts match strains to individual needs, avoiding unverified claims. Always consult professionals for personalized advice.
Ready to optimize gut health? Connect via WhatsApp at +60123822655 (Mon–Fri, 9:30am–6:30pm). Your journey to better digestion begins here.
FAQ
How do beneficial bacteria withstand harsh stomach conditions?
Certain strains produce protective enzymes like F0F1-ATPase, which neutralizes acidity by pumping protons out of cells. Others form biofilms or rely on food buffers for enhanced survival.
Does glucose improve bacterial viability in acidic environments?
Yes. Research shows sugars fuel ATP production through glycolysis, helping lactic acid bacteria maintain energy levels when pH drops below 3.0.
Which strains demonstrate the highest acid resistance?
Lactobacillus rhamnosus GG and Bifidobacterium animalis show exceptional durability, with some studies reporting 80-90% survival rates after 90 minutes at pH 2.0.
Why does meal timing affect supplement effectiveness?
Consuming with food—especially dairy or high-fiber options—creates a protective matrix that reduces gastric acid exposure by 30-50% compared to empty-stomach intake.
Are enteric coatings necessary for all supplements?
Not for resilient strains like Bacillus coagulans, which forms protective spores. However, coatings help delicate microorganisms survive upper gastrointestinal transit intact.
How do bile salts impact viability after stomach passage?
Adaptive species modify cell membrane lipids to resist bile’s detergent effects, with certain Lactobacillus strains showing 70% higher duodenal survival than non-adapted counterparts.
Can these microorganisms support H. pylori treatment?
Clinical trials indicate specific strains reduce bacterial load by 40-60% when used alongside antibiotics, likely through competitive exclusion and mucosal barrier reinforcement.
What evidence confirms successful intestinal colonization?
PCR testing of stool samples provides accurate viability data, unlike home tests. Look for studies measuring CFU counts before and after gastrointestinal transit.

Khloe Tan
Khloe Tan is a Certified Nutritionist, Corporate Wellness Trainer, and Holistic Health Specialist with over 15 years of experience in the health and wellness industry. She has delivered more than 100 talks nationwide, inspiring and educating diverse audiences on nutrition, lifestyle, and sustainable wellness. Her work has positively impacted over 3,000 lives, and she continues to champion holistic approaches to well-being in both corporate and personal settings.
Feature Product
-
Hydrogen Water FIlter/Generator
H2zen Portable (White/ Blue)
RM2,600.00 Add to cart Buy NowRated 0 out of 5





