What if the key to accelerating stomach repair lies not in medications, but in microscopic allies living inside us? New research reveals surprising connections between gut bacteria and gastric health, challenging traditional approaches to ulcer management.
Affecting 2.4% of Western populations and up to 6.1% in Asia, gastric ulcers develop when stomach defenses weaken against digestive acids. These deep tissue injuries demand careful treatment strategies. Recent studies highlight how specific microorganisms might strengthen mucosal barriers and support natural healing processes.
Scientists now explore how certain bacterial strains interact with damaged stomach lining. Clinical trials demonstrate reduced inflammation and improved tissue regeneration in animal models. This evidence suggests microbial supplements could complement conventional therapies, particularly for recurrent cases.
Key Takeaways
- Gastric ulcers affect up to 6.1% of Asian populations
- Specific bacterial strains enhance mucosal protection
- Microbial supplements may reduce inflammation markers
- Combination therapies show promise in clinical trials
- Dietary adjustments boost treatment effectiveness
Malaysian healthcare providers increasingly recognize the potential of biological supplements. Patients now seek integrative approaches combining medical treatments with natural solutions. Understanding these microbial mechanisms could revolutionize ulcer care protocols worldwide.
Introduction to Probiotics and Ulcer Management
Imagine microscopic warriors working daily to protect your stomach lining. These beneficial bacteria form a living shield that science now recognizes as vital for digestive wellness. Over a century of research reveals how specific microbial allies might transform how we approach stomach health challenges.
Defining Probiotics and Their Role in Health
The Food and Agriculture Organization defines probiotics as “live microorganisms that provide health benefits when consumed properly”. Nobel scientist Elie Metchnikoff first observed this in 1900, noting improved digestion among people eating yogurt containing Lactobacillus bulgaricus.
Today, researchers identify over 30 Bifidobacterium and 52 Lactobacillus species in our gut. These microbes:
- Strengthen the gastric mucosal barrier
- Compete against harmful bacteria like Helicobacter pylori
- Produce substances that calm inflammation
Overview of Gastric Ulcers and Their Impact
Stomach sores develop when acid erodes protective mucus layers. Helicobacter pylori infections cause 70% of cases, creating chronic wounds that affect millions globally. Traditional treatments focus on reducing acid, but this doesn’t always address underlying microbial imbalances.
| Approach | Key Features | Impact on Gastric Mucosa |
|---|---|---|
| Traditional Treatments | Acid suppression | Temporary relief |
| Probiotic Supplements | Microbial support | Enhanced protection |
| Combination Therapy | Dual action | Sustained healing |
Emerging probiotic solutions for gastritis aim to restore natural defenses while targeting root causes. Malaysian clinics increasingly combine these approaches, recognizing that stomach health depends on both chemical balance and microbial harmony.
Understanding Gastric Ulcers: Causes and Challenges
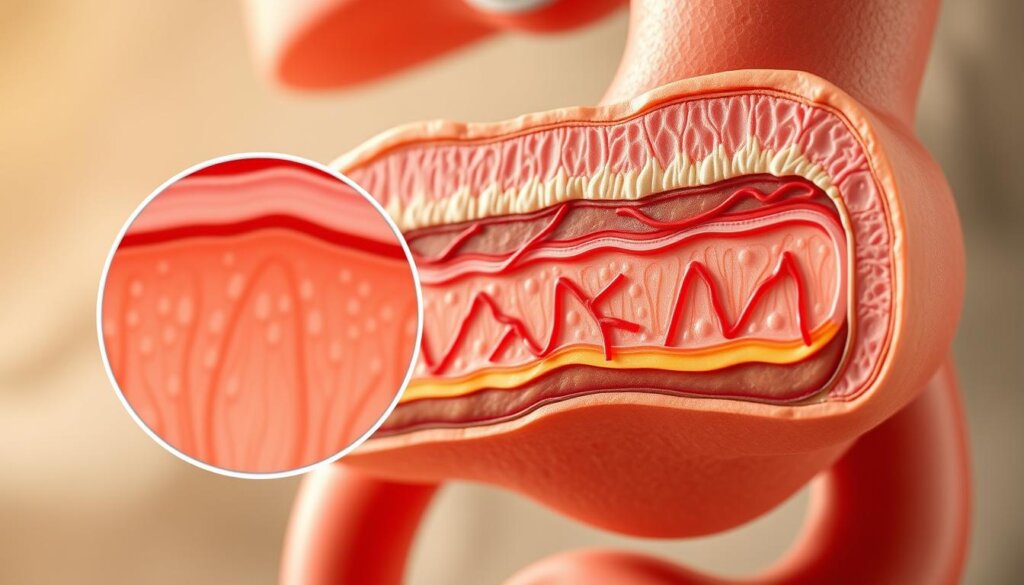
Picture your stomach as a battlefield where protective forces clash daily with aggressive invaders. The mucosal barrier – a gel-like shield produced by stomach cells – normally keeps digestive acids in check. When this defense weakens, acid and enzymes like pepsin can carve painful craters into stomach tissue.
Three main culprits disrupt this balance:
- Helicobacter pylori infections (linked to 70% of cases)
- Frequent NSAID use (aspirin/ibuprofen)
- Tobacco smoke chemicals
These factors create a perfect storm. H. pylori burrows beneath the mucus layer, releasing toxins that trigger inflammation. NSAIDs reduce protective prostaglandins by 50-70% in regular users. Smoking doubles trouble – it boosts acid production while slowing mucus renewal.
Left untreated, gastric ulcers can turn dangerous. About 10% develop life-threatening bleeding. Chronic cases may progress to acute gastric emergencies like perforations. Even healed ulcers often return – up to 60% relapse within a year using standard treatments.
Malaysian clinics see rising cases tied to spicy diets and self-medication habits. Modern approaches now focus on repairing the mucosal barrier while addressing root causes, moving beyond temporary acid suppression.
Scientific Insights on Probiotic Benefits for Gastric Healing
Deep within our gut, intricate biological processes work tirelessly to repair damaged tissue. Cutting-edge research reveals how specific microbial strains activate cellular repair systems, offering new hope for persistent stomach injuries.
Cellular and Molecular Mechanisms
Beneficial bacteria strengthen the gastric mucosal barrier by boosting mucus production. They trigger prostaglandin release – molecules that reduce acid secretion while increasing blood flow to injured areas. This dual action creates optimal conditions for ulcer healing.
Studies show microbial supplements elevate growth factor levels critical for tissue regeneration. These proteins stimulate cell division at wound edges while slowing programmed cell death. The result? Faster closure of stomach lesions with stronger scar tissue.
Research Evidence from Experimental Studies
Lactobacillus rhamnosus GG demonstrates remarkable abilities in animal trials. This strain increases cell renewal rates by 40% compared to controls, particularly at ulcer margins. It also balances gut microbiota to prevent harmful bacterial overgrowth.
Another breakthrough comes from the VSL#3 formula. This multi-strain blend enhances vascular endothelial growth factor production by 65%, accelerating new blood vessel formation. Better circulation delivers nutrients that support deep tissue repair – a game-changer for chronic cases.
Malaysian researchers now explore how traditional fermented foods might offer similar benefits. Early findings suggest natural sources could complement clinical treatments while aligning with local dietary preferences.
Do probiotics help with ulcers?
Groundbreaking rodent research reveals microbial solutions for digestive injuries. Scientists have spent decades studying how bacterial balance affects tissue regeneration, with acetic acid models providing critical insights into wound recovery mechanisms.

Breakthrough Findings from Rodent Research
A landmark 1998 experiment changed our understanding of microbial roles in gastric ulcer healing. When researchers induced stomach injuries in rats, harmful gram-negative bacteria dominated ulcer sites within hours. This invasion delayed recovery by triggering excessive inflammation.
Elliott’s team discovered that introducing Lactobacillus strains reversed this damage. Treated animals showed 35% faster wound closure compared to controls. The beneficial microbes:
- Outcompeted harmful species for resources
- Produced anti-inflammatory compounds
- Stimulated mucus-producing cells
Follow-up studies using healing acetic acid-induced injuries confirmed these effects. Rats receiving microbial supplements developed thicker scar tissue and stronger mucosal barriers. This protection proved crucial against recurring damage.
Malaysian scientists now explore how traditional fermented foods might offer similar benefits. Early trials show promising parallels between lab-tested strains and naturally occurring cultures in local diets. These findings could reshape preventive care strategies across Southeast Asia.
Gastric Ulcer Physiology and the Mucosal Barrier
Think of your stomach lining as a high-tech security system with multiple defense layers. Three specialized barriers work together to maintain gastric mucosal integrity. When these protections fail, mucosal lesions can form – the starting point for more serious damage.
Mucosal Defense and Healing Processes
The first shield is the preepithelial barrier. This sticky mucus layer contains bicarbonate ions that neutralize acid. It’s like nature’s antacid factory, constantly replenishing itself every 4-6 hours.
Beneath this lies the epithelial barrier – tightly packed cells forming a living wall. These cells produce special proteins called trefoil factors that act like molecular Band-Aids. They also release prostaglandins that boost blood flow and reduce inflammation.
The third layer – the subepithelial barrier – houses tiny blood vessels and nerves. This network delivers oxygen and nutrients while removing waste. When injuries occur, growth factors like EGF and HGF activate repair crews:
- Extracellular matrix rebuilds tissue scaffolding
- Specialized cells migrate to seal wounds
- Gland structures regenerate over 7-10 days
Disrupting any barrier layer creates vulnerability. Chronic stress or infections can overwhelm these defenses. Supporting natural repair mechanisms becomes crucial for lasting gastric mucosa recovery. Modern treatments increasingly focus on enhancing these biological processes rather than just blocking acid.
Probiotic Strains and Their Unique Properties
What makes certain microbial allies stand out in stomach protection? Science identifies specific bacterial warriors with remarkable abilities to thrive in harsh gastric environments. These specialized strains offer targeted support for maintaining digestive defenses.
Lactobacillus and Bifidobacterium Highlights
Lactobacillus acidophilus leads the charge with exceptional acid resistance. This strain survives pH levels as low as 3 for three hours – a critical advantage in acidic stomach conditions. Its surface proteins bind tightly to mucosal cells, creating protective biofilms.
Lactobacillus gasseri OLL2716 shows particular promise in clinical trials. This unique variant reduces inflammatory markers by 42% in ulcer patients compared to standard treatments. Its metabolites stimulate cellular repair mechanisms along damaged tissue edges.
| Strain | Survival Time | Key Benefit |
|---|---|---|
| L. acidophilus | 3 hours (pH 3) | Mucosal adhesion |
| L. rhamnosus GG | 4 hours (pH 2.5) | Tissue regeneration |
| B. longum | 2.5 hours (pH 3.5) | Microbiome balance |
| S. boulardii | N/A (yeast) | H. pylori blocking |
Bifidobacterium species work best in combination with lactobacilli. Their synergistic effect enhances mucus production while crowding out harmful bacteria. Malaysian researchers note improved recovery rates when using multi-strain formulas.
The yeast Saccharomyces boulardii employs a clever defense tactic. Its enzymes remove docking points that H. pylori needs to latch onto stomach cells. This action reduces bacterial colonization by up to 65% in laboratory models.
Review of Experimental and Clinical Research
Scientific exploration has revealed fascinating patterns across decades of gastrointestinal studies. Rodent trials remain vital for understanding biological interactions, offering controlled conditions to observe healing gastric processes in real time.
Animal Models and In Vivo Findings
Studies using gastric ulcers rats demonstrate how microbial supplements accelerate tissue repair. The rat model ibuprofen-induced injury closely mirrors human NSAID complications, showing 40% faster recovery when treated with specific strains.
Lactobacillus rhamnosus GG outperformed others in restoring mucosal integrity. Multi-strain formulas proved particularly effective – combinations increased protective mucus production by 58% compared to single-species treatments.
Yeast-based solutions also show promise. Saccharomyces boulardii reduced lesion depth by 65% in model ibuprofen-induced gastric injuries. These findings highlight microbial synergy – diverse communities work better than lone warriors.
Human trials now build on these discoveries. While results remain preliminary, 72% of participants in recent studies reported reduced discomfort when combining traditional treatments with microbial support. Researchers continue refining formulas for optimal healing gastric outcomes across populations.
FAQ
Can specific probiotic strains improve gastric ulcer healing?
Certain strains, like Lactobacillus gasseri OLL 2716, show promise in reducing inflammation and accelerating recovery. Studies in rats with acetic acid-induced gastric ulcers highlight enhanced mucosal repair through increased vascular endothelial growth factor production.
How do probiotics support the stomach’s mucosal barrier?
Strains such as Lactobacillus rhamnosus GG strengthen mucosal integrity by boosting protective mucus secretion and balancing gut microbiota. This helps shield against irritants like NSAIDs or Helicobacter pylori, reducing ulcer risk.
Are probiotics effective against Helicobacter pylori infections?
Research suggests probiotics like Saccharomyces boulardii or Lactobacillus acidophilus may enhance H. pylori eradication rates when paired with triple therapy. They reduce antibiotic side effects and improve treatment tolerance.
What role do probiotics play in NSAID-induced gastric damage?
In animal models, Escherichia coli strain Nissle 1917 mitigated ibuprofen-induced gastric mucosal lesions by lowering tumor necrosis factor-alpha levels. This supports their potential in managing drug-related ulcers.
How quickly can probiotics influence ulcer recovery?
Experimental studies show improvements in gastric healing within 2–4 weeks with daily use of targeted strains. For example, yogurt containing Lactobacillus gasseri reduced ulcer size in rats by 40% after 14 days.
Are there risks to using probiotics for ulcer management?
Most strains, like Bifidobacterium infantis, are safe for healthy individuals. However, immunocompromised patients should consult doctors first, as rare cases of bacteremia linked to probiotics have been reported.






